Sorry…this post is going to be a TL,DR (too long, didn’t read) for many people so here is the summary:
There are only two studies that are prospective, randomized trials of epidural medications and their effects on breastfeeding. The first, by Beilin and friends (et. al.) found no association between epidural medications and breastfeeding difficulties (as assessed by both mom and a lactation consultant) at 24 hours after birth. They found that women who received more than 150 micrograms of epidural fentanyl total were more likely to have stopped breastfeeding at 6 weeks but the drop out rate from the study was high (11%) and the significance of this finding really needs to be tested in another study. Stopping breastfeeding at 6 weeks also correlated with maternal reports of breastfeeding problems at 24 hours which suggests that those moms that report difficulties could benefit from more lactation support in the postpartum period.
The second study, an RCT by Wilson et al, provides good evidence that epidurals do NOT have an effect on breastfeeding.
Other studies in this area are either cohort or retrospective and do not provide any compelling evidence that breastfeeding is hindered by epidurals.
Blaming epidurals for lack of breastfeeding success is barking up the wrong tree. With supportive policies in place in the hospital women who want an epidural to decrease their labour pain will be able to breastfeed with the same success as women who chose “natural” childbirth.
Most of the studies I am about to discuss are available, free of charge on the internet. The rest I got from my University library…for those of you who are interested but who don’t have access, I am happy to email PDFs.
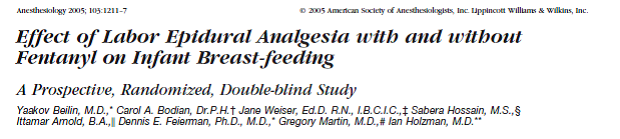
Prior to Beilin et al, studies looking at the effect of labour epidurals were either retrospective, or non-randomized prospective studies. Theirs was the first prospective randomized trial looking at this important question.
This study comes from the Mount Sinai School of medicine in New York and was published in a well-regarded peer-reviewed journal in 2005.
The authors took a group of pregnant women who had already had at least one baby who they had breastfed for 6 weeks or more and who planned to breastfeed their next baby also. When they requested an epidural during labour they were assigned into one of three groups:
– Local anesthetic only, no epidural narcotic
– Local anesthetic plus up to 150 micrograms of epidural fentanyl total for the duration of the epidural infusion
– Local anesthetic plus no cap on the micrograms of epidural fentanyl
Women who had IV or IM narcotic during their labour were excluded as were those that had a C/S. If a woman couldn’t be made comfortable, additional medications (including more fentanyl) were given by the anesthesiologist. The groups were analyzed two ways: an intention to treat analysis was used keeping all women in their assigned groups, and then a second analysis was done by grouping the women into three groups based on the actual amount of fentanyl they had received. The trial was double blinded – the woman and those assessing breastfeeding did not know which medications had been used in the epidural.
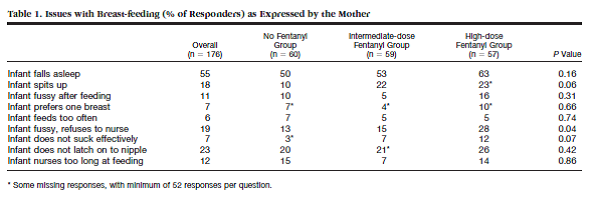
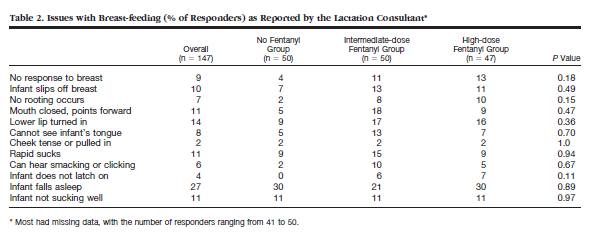
The outcomes studied were perceived problems breastfeeding by the women themselves, problems observed by lactation consultants and number still breastfeeding at 6 weeks.
When breastfeeding was assessed at 24 hours by moms and lactation consultants, no differences were found between the groups with the exception of “infant fussy, refuses to nurse” reported by moms (p = 0.04). But with 21 statistical tests, it would be more shocking if none of them proved to be statistically significant. With a p value of 0.05 set as significant, one out of every 20 comparisons will be significant by chance alone.
21 women couldn’t be reached at 6 weeks or chose not to participate. At 6 weeks, it was less likely (statistically significant) that women in the high dose fentanyl group were still breastfeeding. All women who stopped breastfeeding cited difficulties breastfeeding as the reason. Interestingly, stopping breastfeeding before 6 weeks correlated with women’s perceived difficulties breastfeeding at 24 hours but not the evaluation by the lactation consultant.
I think this study is interesting but not definitive. The finding that higher dose epidural fentanyl was associated with cessation of breastfeeding at 6 weeks is interesting but doesn’t prove causation. It wasn’t reported in the paper which groups those 21 women who didn’t respond/ chose not to participate in the 6 week survey belonged to. If they all came from one group that would probably throw the results off. In general, when there is a high drop out from a study, the results become less reliable. What if those 21 women didn’t answer the phone because they were busy breastfeeding? What if those 21 women had to go back to work and so weren’t available for phone calls or able to continue breastfeeding because of poor maternity leave policies?
How will this change my practice? First, I think it’s great news that no differences were apparent between groups in terms of breastfeeding difficulties at 24 hours. In terms of the results at 6 weeks, there might be an association with larger doses of fentanyl. That reiterates to me the importance of choosing to give the lowest doses possible to achieve maternal comfort in my labour epidurals (always a good idea). We add fentanyl to bupivacaine (or another local anesthetic) because that way we can achieve more pain relief with less motor block. Less motor block allows women to push and change positions (and sometimes walk) and potentially avoid forceps or other assisted delivery. I would love to see another study designed specifically to look at this issue and I would need to see a well-conducted positive study before I gave up or severely restricted fentanyl in epidurals. The other thing that kind of bothers me is that, although we know some fentanyl is transferred to the fetus during labour, at the doses used in this study, there wasn’t a measurable difference in infant behaviour after birth. That leaves me to question…what could the possible mechanism be between larger fentanyl doses in labour and early cessation of breastfeeding? If we can’t think of a biologically plausible mechanism, could this effect have occurred by chance alone?
The association between breastfeeding difficulties perceived by mom and giving up breastfeeding at 6 weeks is just as interesting. Maybe switching to formula and bottle feeding by 6 weeks has nothing to do with fentanyl at all but tons to do with maternal expectations. Maybe women who express some dissatisfaction with how nursing is going in the hospital should be offered more intensive lactation consultant help, follow-up and encouragement. There are so many “maybes” here that another study is warranted to answer this question. Remember, associations do NOT prove causation…but they should make us sit up and take notice and do some further investigation!
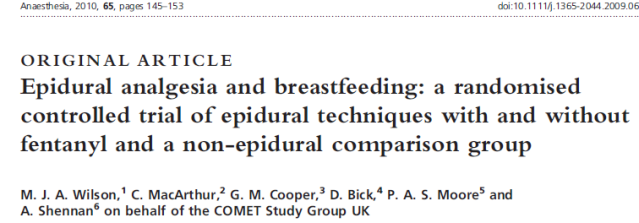
The only other RCT on this subject is by Wilson et al, it was published 5 years later in 2010:
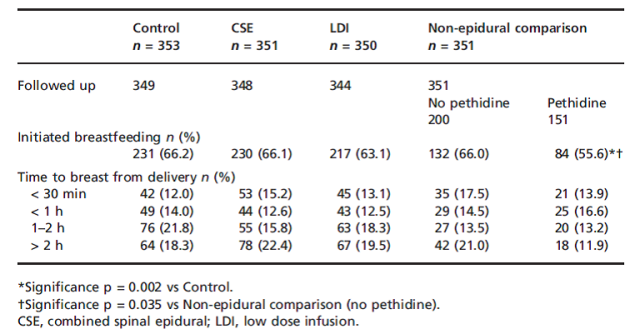
This study comes from the COMET (Comparative Obstetric Mobile Epidural Trial) data. This trial was done in the late 1990s to investigate the use of lower dose epidurals for labour pain relief and their possible effects on the success of vaginal delivery (btw, they found that the newer, lower dose techniques were NOT associated with greater rates of instrumented or Caesarian delivery). At the time, they also collected information on breastfeeding. The paper by Wilson et al looks at four groups of women having their first baby. Women who requested epidurals were randomized to three groups: a “high” dose (HDI) epidural group (bupivacaine only, 353 women), a low dose (LDI) epidural group (bupivacaine and fentanyl, 350 women) and a combined spinal-epidural (CSE) group (bupivacaine and fentanyl, 351 women). The fourth group was made up of women who didn’t have an epidural (351 women) who were matched to the trial women by mode of delivery and ethnicity. Drop out rates over the 12 months of follow-up were similar between groups:
|
Group |
Number recruited | Number assessed at 24 h post partum | Number assessed at 12 mo |
| HDI | 353 | 349 | 262 |
| LDI | 350 | 344 | 263 |
| CSE | 351 | 348 | 267 |
| Control/ non-Epi | 350 | 344 | 251 |
When they looked at the time to initiate breastfeeding, about 2/3rds of women overall initiated breastfeeding which is interesting given that the rate of breastfeeding initiation in the UK where the study was done was reported to be 76%. The only significant difference between groups was that women from the control group who had IV or IM pethidine (Demerol) were less likely to initiate breastfeeding. Time to breastfeeding initiation was similar between the groups. Women were more likely to start breastfeeding if they were non-white and older.
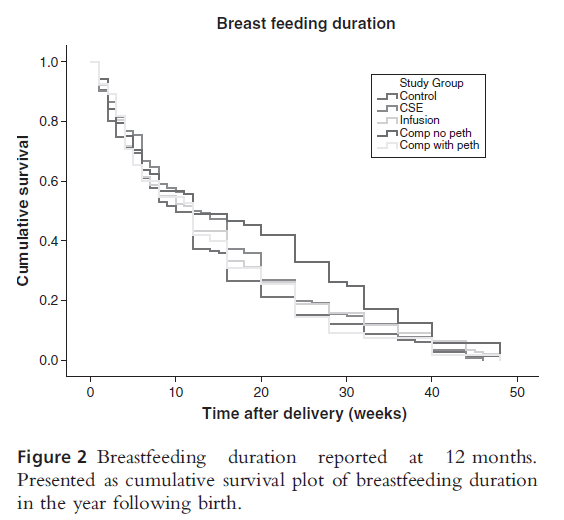
At the 12 month follow-up, there were no differences between the groups in terms of breastfeeding duration. Although the curves below look slightly different, the confidence intervals overlap and the “differences” aren’t statistically significant. Does it strike you as funny that they label “still breastfeeding” as “survival?” I had a good chuckle over that.
I think this trial provides good evidence that there is NO effect of modern low dose epidural infusions which include fentanyl on breastfeeding initiation or duration. Women without labour epidurals did not initiate breastfeeding at greater rates than those with epidurals.
Next, let’s look at this 2006 cohort study by Torvaldsen et. al.
This study was done in Australia. Women were enrolled in the study if they gave birth to a live infant and were over the age of 16. Women were recruited who had births in public and private hospitals, a birth center as well as at home. These women were given questionnaires at 4 days, 8, 16 and 24 weeks after the birth to complete. 1961 women were eligible but only 70% of those approached agreed to participate in the study. 92% of women who started the study actually completed the 24 week questionnaire which is an amazingly low drop-out rate.
33% of the women had epidurals but all of them had pethidine prior to initiation of their epidurals. Did the hospital have some sort of policy that a woman had to try pethidine prior to allowing an epidural? This is a very curious finding indeed!
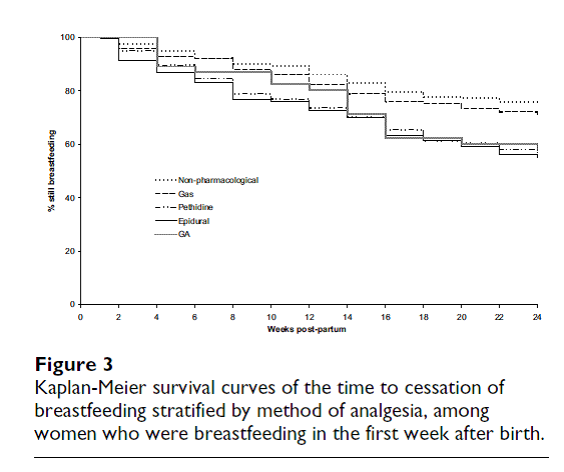
It is encouraging that fully 93% of women were breastfeeding in the first week postpartum and 60% were breastfeeding at 24 weeks. Of the women who were not breastfeeding in the first week, 48% of them had not planned to breastfeed in the first place. It is interesting to me that the authors reported factors associated with full breastfeeding vs partial breastfeeding. Partial breastfeeding in the first postpartum week was associated with increased risk of stopping breastfeeding by week 24 in this study. Although it seemed that the use of either an epidural or a general anesthetic was associated with partial breastfeeding in the first week, after adjusting for vaginal birth and parity, no statistically significant difference was found…although the authors still stated in their discussion and abstract that a difference was present (once again proving that you can’t just read the abstract).
Women who had an epidural or pethidine were more likely to stop breastfeeding by 24 weeks (6 mo). Since all women who had an epidural also had pethidine, it’s unclear to me how these two groups were different. Although they tried to do an analysis of “epidural only” vs “epidural with pethidine,” all of the women who had an epidural without pethidine were women who had planned Caesarian sections. Since we know that mode of delivery correlates breastfeeding rates I think this analysis adds little value. We still don’t know if it was the epidural or the pethidine that interfered with breastfeeding. Judging by the more robust results of the RCT by Wilson et al, I’m inclined to think it was the pethidine…The other difficulty I have when interpreting this cohort study, is that there was no standardized epidural dosage or solution.
Here’s another prospective cohort study:
This was a retrospective study of 105 women who gave birth in a hospital in Toronto. To be included in this study you had to have already successfully breastfed an infant and be intending to breastfeed this one too. This was in an attempt to replicate the results by Beilin et. al. The primary outcome was breastfeeding cessation at six weeks. They excluded women who had received opioids or nitrous oxide prior to epidural analgesia. This study may not be widely generalizable…the breastfeeding rate was 96% and the median maternity leave was 12 months! In addition, the median length of prior breastfeeding for these women was 11.5 months so they might comprise a group of super-breastfeeders.
At six weeks, four women had stopped breastfeeding. One of these had received > 150 micrograms of fentanyl while three had received less. These results are the opposite of Beilin et. al. although the study by Wieczorek et. al. is significantly less robust. The numbers were very small and it wasn’t randomized. The most we can say about this study is best said by the authors themselves:
Next, let’s look at the retrospective observational study, Jordan et. al published in BJOG in 2009.
Jordan et. al. is a great example of a data dredge…now there is nothing inherently wrong with a data dredge as long as you interpret the results with caution…They looked at the Cardiff Births survey data from Wales, UK, examining the results of 48 366 births of single infants at term that occurred between 1989 and 1999. Using regression analysis, they looked at factors associated with partial or complete breastfeeding at 48 hours vs. bottle/ formula feeding. And they found a ton!!
They found associations with oxytocin (10 U IM used routinely to decrease postpartum hemorrhage), ergotamine, epidurals, social class, induction, C-section, parity, maternal age….The great thing about this paper is that the authors, being astute, mention several times that these associations don’t prove anything and they advocate for studies specifically designed to look at the effect these factors might have on breastfeeding. Data dredging (retrospective) studies are great for hypothesis generating…not so great for offering conclusions.
I’m not sure why a natural childbirth advocate would take these author’s data out of context and subscribe more importance to it than they themselves do…(tongue firmly in cheek):
“Considering drugs used in labor generally, Jordan, et al (2009) provide some evidence that drug use in labor and birth has an impact on breastfeeding rates at 48 hours postpartum. (Of course, when women have already given up on breastfeeding two days after giving birth, it’s unlikely that they will re-establish breastfeeding later, even though this might be possible.) However, although Jordan et al’s conclusions are fairly clear, we also need to take into account the fact that many anesthesiologists wouldn’t accept these researchers’ conclusions simply because their data is retrospective” (Sylvie Donna, Science and Sensibility).
Another retrospective study (published as a letter only) from Glasgow from V Uppal and SJ Young:
This study retrospectively looked at 13741 deliveries and a woman’s intention to breastfeed at hospital discharge. 5652 women intended to breastfeed while 7668 women intended to exclusively formula feed. Again, given the low rate of intention to breastfeed overall, I think this population may not be representative of most communities. Factors that were found to be associated with breastfeeding intention included older maternal age, and being a non-smoker. Factors associated with choosing to formula feed included a non-white ethnicity, multiparity, opioids during labour and having a Caesarian section. Epidurals were not associated with breastfeeding at all in this study. Again, these associations are interesting, but don’t tell us anything about causation…they are simply fodder for future prospective controlled trials.
I’m fairly confident (based on the studies by Beilin and Wilson et. al.) that epidurals do not have an effect on the establishment of breastfeeding or the duration of breastfeeding. If I’m wrong and such an effect exists, I think it ‘s pretty small (would require a trial with hundreds of women in each arm) and likely to be overcome by social factors and lactation support.
I’m not going to review the basic science articles right now. I don’t see a compelling reason given that we have good clinical trial evidence that shows epidurals don’t affect breastfeeding significantly.
Unfortunately, I can’t access the following articles at this time and will have to revisit them later:
Gizzo S, Di Gangi S, Saccardi C, Patrelli TS, Paccagnella G, Sansone L, Barbara F, D’Antona D, Nardelli GB. Epidural Analgesia During Labor: Impact on Delivery Outcome, Neonatal Well-Being, and Early Breastfeeding. Breastfeed Med. 2011 Dec 13. [Epub ahead of print]
Henderson JJ, Dickinson JE, Evans SF, McDonald SJ, Paech MJ. Impact of intrapartum epidural analgesia on breast-feeding duration. Aust N Z J Obstet Gynaecol. 2003 Oct;43(5):372-7.
Just for fun, I read the review articles to see if my reading of the primary literature agreed with these experts. Both Devroe and Loubert agree with me that current evidence does not support any link between epidurals and breastfeeding. Reynolds also agrees but she also points out that some of the hospitals where studies were done had policies for women who had epidurals that were not conducive to breastfeeding including separating the women from their infants in the first hours after birth. That is a significant confounder! Pandya says that the only well conducted trials don’t support a link while the studies that suggest an association between epidurals and not breastfeeding are over-represented in the media.
Blaming epidurals for lack of breastfeeding success is barking up the wrong tree. With supportive policies in place in the hospital women who want an epidural to decrease their labour pain will be able to breastfeed with the same success as women who chose “natural” childbirth.
REFERENCES
RCTS
Beilin Y, Bodian CA, Weiser J, Hossain S, Arnold I, Feierman DE, Martin G, Holzman I. Effect of labor epidural analgesia with and without fentanyl on infant breast-feeding: a prospective, randomized, double-blind study. Anesthesiology. 2005 Dec;103(6):1211-7.
Wilson MJ, MacArthur C, Cooper GM, Bick D, Moore PA, Shennan A; COMET Study Group UK. Epidural analgesia and breastfeeding: a randomised controlled trial of epidural techniques with and without fentanyl and a non-epidural comparison group. Anaesthesia. 2010 Feb;65(2):145-53. Epub 2009 Nov 12.
PROSPECTIVE STUDIES (NON RCT)
Torvaldsen S, Roberts CL, Simpson JM, et al. Intrapartum epidural analgesia and breastfeeding: a prospective cohort study. International Breastfeeding Journal, 2006,Dec11;1:24
RETROSPECTIVE
Jordan S, Emery S, Watkins A, Evans JD, Storey M, Morgan G. Associations of drugs routinely given in labour with breastfeeding at 48 hours: analysis of the Cardiff Births Survey. BJOG. 2009 Nov;116(12):1622-9; discussion 1630-2. Epub 2009 Sep 1.
Wieczorek PM, Guest S, Balki M, Shah V, Carvalho JC. Breastfeeding success rate after vaginal delivery can be high despite the use of epidural fentanyl: an observational cohort study. Int J Obstet Anesth. 2010 Jul;19(3):273-7. Epub 2010 Jun 2.
Uppal V, Young SJ. Smoking and ethnic group, not epidural use, determine breast feeding outcome. Anaesthesia. 2010 Jun;65(6):652. No abstract available.
REVIEWS
Devroe S, De Coster J, Van de Velde M. Breastfeeding and epidural analgesia during labour. Curr Opin Anaesthesiol. 2009 Jun;22(3):327-9. Review.
Loubert C, Hinova A, Fernando R. Update on modern neuraxial analgesia in labour: a review of the literature of the last 5 years. Anaesthesia. 2011 Mar;66(3):191-212. doi: 10.1111/j.1365-2044.2010.06616.x. Review.
Reynolds F. The effects of maternal labour analgesia on the fetus. Best Pract Res Clin Obstet Gynaecol. 2010 Jun;24(3):289-302. Epub 2009 Dec 11. Review.
Pandya ST. Labour analgesia: Recent advances. Indian J Anaesth. 2010 Sep;54(5):400-8.
UNKNOWN
Gizzo S, Di Gangi S, Saccardi C, Patrelli TS, Paccagnella G, Sansone L, Barbara F, D’Antona D, Nardelli GB. Epidural Analgesia During Labor: Impact on Delivery Outcome, Neonatal Well-Being, and Early Breastfeeding. Breastfeed Med. 2011 Dec 13. [Epub ahead of print]
Henderson JJ, Dickinson JE, Evans SF, McDonald SJ, Paech MJ. Impact of intrapartum epidural analgesia on breast-feeding duration. Aust N Z J Obstet Gynaecol. 2003 Oct;43(5):372-7.



“what could the possible mechanism be between larger fentanyl doses in labour and early cessation of breastfeeding?”
I wonder if the common factor is simply: mother’s pain sensitivity / threshhold? Perhaps women who experience a great deal of pain in labor (and so need a higher does of meds) also experience more pain / discomfort than normal with nursing and so are less motivated to continue?
I had an epidural, and trouble breast feeding in the hospital- little boy wouldn’t stop crying. But as soon as we were home all of our bf-ing issues disappeared and I became a serious over producer.
I have a friend who has 4 children, the first two non- medicated the last two medicated. Her first was seriously premature and never properly latched, second was perfect and didn’t latch- at 3 they realized she was tongue tied. Her second two she had some breast feeding success- and she was COMMITTED. Her problem ended up being lack of supply/ a horrendous mysterious breast infection.
Sometimes I think it’s luck. If I had had the same problems she had I never would have persevered as long as she did. I do think breast feeding is too complicated to point to a single cause for failure or success. That said, I enjoyed reading the studies and hope they will lead to more.
Huh! I’m reading your blog backwards, so please therefore disregard a previous comment requesting a post on this topic exactly! Thanks!!